Multi-Energy computed tomography (MECT) for radiation therapy
Jessica Miller, Ph.D., DABR
University of Wisconsin – Madison, USA![]()
Increasing role of MECT in RT simulation
Nearly all patients treated with radiation therapy (RT) receive a computed tomography (CT) simulation scan for treatment planning purposes. Multi-energy CT (MECT) allows for the reconstruction of supplementary information during the CT simulation process, such as relative electron density and effective atomic number information, virtual monoenergetic images, and material decomposition. The additional information gained through MECT has the potential to aid in several aspects of the RT process.
Improving dose calculation accuracy through MECT imaging has been an area of interest for several RT modalities. Electron density and effective atomic number images provide a unique benefit for proton-therapy dose calculations, where the stopping power ratio is directly proportional to the effective atomic number [1]. Effective atomic number information can also aid in dose calculation accuracy for low-energy brachytherapy, where the photo-electric interaction probability increases. In addition, virtual non-iodine images allow for the reconstruction of contrast and non-contrast images from a single CT acquisition, reducing uncertainties in dose calculation due to image registrations for images acquired separately and obviating the need for density overrides in areas of iodine uptake.
Visualization of soft tissue disease can be challenging with conventional CT imaging. MECT virtual monoenergetic images (VMIs) allow for the optimization of the beam energy for visualization purposes. Low-energy VMIs can help delineate tumor from healthy parenchyma, particularly in areas of iodine uptake [2]. Several studies have also demonstrated improvements in contrast to noise ratios for organs at risk. Conversely, high-energy VMIs benefit from lower image noise and a reduction in image artifacts caused by metals and beam hardening. In addition, several studies have demonstrated improvements in prediction models when incorporating multiple MECT images. Changes in texture features and radiomics analysis across multiple MECT images may reflect tissue-specific characterizations and improve treatment response assessment [3].
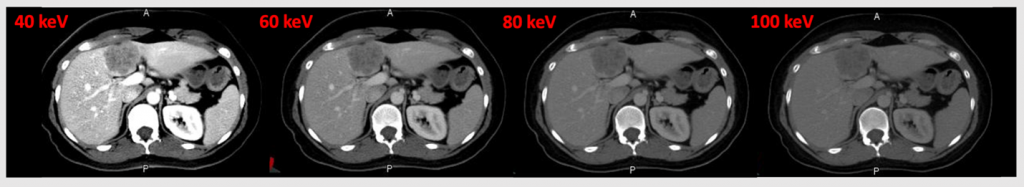
An example of virtual monoenergetic images reconstructed for a patient who was treated for metastatic rectal adenocarcinoma. The low-energy images, demonstrate greater contrast between areas of differentiating iodine uptake, such as the tumor and surrounding liver parenchyma.
Functional tissue segmentation is another critical complement to improving quality of care for RT patients. MECT images can provide visualization of functional tissue for several organs including lung, liver, and bone marrow. Late-phase iodine maps can highlight areas of non-functioning liver due to low hepatic venous outflow caused by scarred or fibrotic tissue [4]. Material quantification of iodine and xenon gas can aid in the delineation of areas of highly perfusing and ventilating lung, respectively [5]. Virtual non-calcium images allow for the visualization of active marrow, which can serve to reduce hematotoxicites for pelvic patients receiving concurrent chemoradiation [6]. As multi-energy CT technology continues to advance and more radiotherapy clinics adopt this technology, the role of MECT in RT simulation is likely to continue to expand and improve the quality of patient care.
References:
[1] N. Peters, P. Wohlfahrt, C. Hofmann, C. Möhler, S. Menkel, M. Tschiche, et al. Reduction of clinical safety margins in proton therapy enabled by the clinical implementation of dual-energy CT for direct stopping-power prediction Radiother Oncol (2022).
[2] Di Maso LD, Huang J, Bassetti MF, DeWerd LA, Miller JR. Investigating a novel split-filter dual-energy CT technique for improving pancreas tumor visibility for radiation therapy. J Appl Clin Med Phys. 2018; 19: 676– 683.
[3] Forghani R, Chatterjee A, Reinhold C, Pérez-Lara A, Romero-Sanchez G, Ueno Y, Bayat M, Alexander JWM, Kadi L, Chankowsky J, Seuntjens J, Forghani B. Head and neck squamous cell carcinoma: prediction of cervical lymph node metastasis by dual-energy CT texture analysis with machine learning. Eur Radiol. 2019 Nov;29(11):6172-6181.
[4] Ohira S, Kanayama N, Toratani M, Ueda Y, Koike Y, Karino T, Shunsuke O, Miyazaki M, Koizumi M, Teshima T. Stereotactic body radiation therapy planning for liver tumors using functional images from dual-energy computed tomography. Radiother Oncol. 2020 Apr;145:56-62.
[5] Zhang LJ, Zhou CS, Schoepf UJ, Sheng HX, Wu SY, Krazinski AW, Silverman JR, Meinel FG, Zhao YE, Zhang ZJ, Lu GM. Dual-energy CT lung ventilation/perfusion imaging for diagnosing pulmonary embolism. Eur Radiol. 2013 Oct;23(10):2666-75.
[6] Magome T, Froelich J, Takahashi Y, Arentsen L, Holtan S, Verneris MR, Brown K, Haga A, Nakagawa K, Holter Chakrabarty JL, Giebel S, Wong J, Dusenbery K, Storme G, Hui SK. Evaluation of Functional Marrow Irradiation Based on Skeletal Marrow Composition Obtained Using Dual-Energy Computed Tomography. Int J Radiat Oncol Biol Phys. 2016 Nov 1;96(3):679-87.

