Is the dose to circulating blood in conformal radiotherapy of concern?

Harald Paganetti, PhD
Massachusetts General Hospital and
Harvard Medical School, Boston
Systemic effects of conformal radiation therapy
In contrast to chemotherapy, radiation therapy has always been seen as a very localized form of cancer therapy, because one tries to eradicate the tumor with a defined prescription dose while minimizing dose to organs at risk.
However, radiation therapy also has systemic implications as radiation has both immune-stimulatory and immune-suppressive effects [1]. The interaction of radiation with the immune system is complex and often difficult to interpret. For instance, radiation has detrimental effects not only on lymphocytes residing within lymphoid organs but also on tumor infiltrating lymphocytes and on circulating lymphocytes in the blood. Most radiation therapy patients develop radiation-induced lymphopenia. Severe lymphopenia has been associated with poor overall survival, occurrence of distant metastases, and disease recurrence. Even though circulating lymphocytes only present ~2-5% of the total lymphocyte population in the body, a correlation of lymphopenia and treatment outcome, due to dose to circulating lymphocytes, has been demonstrated. Therefore, during fractionated radiation therapy, depletion of circulating lymphocytes originates to a large extend from damaging or killing lymphocytes when irradiating blood vessels.
The number of radiation therapy options for cancer patients has increased significantly in recent years. For instance, volumetric modulated arc therapy (VMAT) is now being used in addition to intensity-modulated radiation therapy (IMRT) and proton therapy (IMPT). These modalities differ in the distribution of the low dose bath to the body outside of the planned target volume and in the overall and local treatment delivery time in a fraction (see figure below).
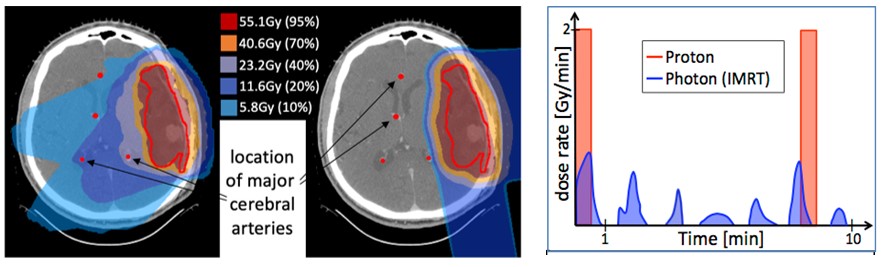
Example dose distribution for an intracranial tumor (left: IMRT; middle: proton therapy). Right: Example time structure of dose delivery for a passively scattered proton therapy and IMRT delivery, respectively.
Dose to circulating lymphocytes is determined by the dose distribution, the fractionation, and the local dose rate relative to the dynamic blood flow. Physicists at several laboratories work on developing computational models to estimate dose to the circulating blood [2]. Consequently, circulating lymphocytes might soon be treated as an organ at risk in treatment planning.
In addition to the impact of hematological dose in radiation therapy, these efforts may also impact the prescription of immunotherapies. Since radiation therapy has both local and systemic effects on the immune system, the combination of radiation therapy with immunotherapy represents a potential tool to maximize immune response. The optimal sequencing of radiation with immunotherapy as well as the optimal radiation modality for combination therapies are being extensively studied [3].
References
[1] Grassberger C; Ellsworth SG; Wilks MQ; Keane FK; Loeffler JS: Assessing the interactions between radiotherapy and antitumour immunity. Nat Rev Clin Oncol. 2019 16(12): 729-745.
[2] Hammi A; Paganetti H; Grassberger C: Modeling intra-cranial blood flow for simualting dose to lymphocytes in radiation therapy treatment regimens. Physics in Medicine and Biology, 2020: 65(5):055008.
[3] Crittenden M; Kohrt H; Levy R; Jones J; Camphausen K; Dicker A; Demaria S; Formenti S: Current clinical trials testing combinations of immunotherapy and radiation. Semin Radiat Oncol, 2015. 25(1): 54-64

